Spinal stenosis is a condition that often manifests subtly but has a profound impact on the quality of life for those it affects. As someone who values the importance of health education, I feel compelled to demystify this condition, often shrouded in technical jargon, and make it more accessible to the layperson. In this comprehensive article, we will delve into the intricacies of spinal stenosis, exploring its causes, recognizing its symptoms, and examining the myriad of treatment options available.
Introduction to Spinal Stenosis
As we embark on this exploration of spinal stenosis, it’s crucial to establish a foundational understanding of the condition. Imagine your spine as a protective tunnel, safeguarding the delicate pathways of your nervous system. Now picture that tunnel gradually narrowing, compressing the nerves within. This is the essence of spinal stenosis – a narrowing of the spaces within your spine, which can lead to nerve irritation and discomfort.
In my journey through the health field, I’ve encountered numerous individuals affected by this condition. Their experiences highlight the importance of raising awareness and understanding the complexities of spinal stenosis. So, let us begin by unraveling the mystery of what exactly spinal stenosis is.
What is Spinal Stenosis?
The term ‘spinal stenosis’ encompasses a variety of scenarios where the spinal canal or the foramina – the small openings through which nerves exit the spine – become constricted. This constriction can occur anywhere along the spine but most frequently affects the neck (cervical) and lower back (lumbar) regions. While some individuals are born with a narrow spinal canal, most cases develop as a part of the aging process.
In my practice, I often describe spinal stenosis as a bottleneck effect that disrupts the normal flow of neurological traffic. This bottleneck can lead to symptoms that range from mild to debilitating, influencing not just one’s physical health but also emotional well-being. Understanding the specific types of spinal stenosis is essential for accurate diagnosis and effective treatment.
Understanding the Spinal Anatomy: Cervical and Lumbar Spinal Stenosis
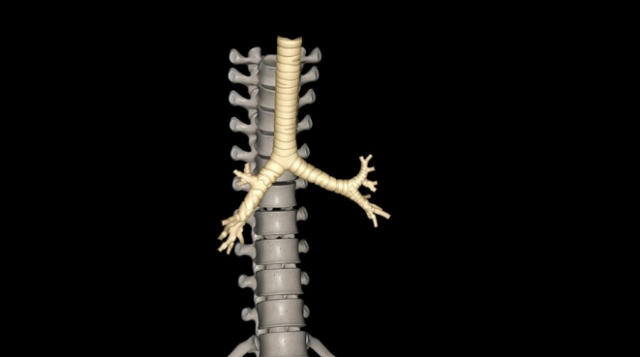
To truly grasp the impact of spinal stenosis, one must first appreciate the complexity of spinal anatomy. The spine is divided into several regions, with the cervical and lumbar areas being most commonly affected by stenosis.
Cervical spinal stenosis occurs in the neck and can have far-reaching effects because it potentially impacts the nerves that control everything from your arms to your diaphragm. Lumbar spinal stenosis, on the other hand, is situated in the lower back. It predominantly affects the nerves that supply your legs and lower body.
In my time working with patients, I’ve observed that lumbar spinal stenosis is more common, but cervical spinal stenosis can often be more serious due to its proximity to the brainstem and spinal cord. Both forms of stenosis can significantly impact daily life, necessitating a deep dive into the root causes of this condition.
Unveiling the Causes of Spinal Stenosis
The origins of spinal stenosis are as multifaceted as the condition itself. It can arise from congenital factors, such as being born with a naturally narrow spinal canal. However, more commonly, it’s the result of age-related changes like osteoarthritis. Over time, wear and tear on the spine can lead to the formation of bone spurs that encroach upon the spinal canal, or thickening of ligaments, which can bulge into the spinal space.
Degenerative conditions, such as spondylolisthesis, where one vertebra slips over another, can also contribute to the narrowing of the spinal canal. Inflammatory diseases, such as rheumatoid arthritis, and trauma to the spine from accidents or injuries can exacerbate or initiate the onset of stenosis.
Herniated discs, which occur when the soft inner core of spinal discs bulges out through a tear in the disc’s tough exterior, can press on the spinal nerves, leading to stenosis-like symptoms. It is this intricate interplay of factors that makes diagnosing and treating spinal stenosis a complex endeavor.
Recognizing Spinal Stenosis Symptoms
Identifying spinal stenosis symptoms is a critical step in managing the condition. These symptoms can be quite variable, often depending on the location and severity of the stenosis. In the lumbar region, symptoms may include pain, weakness, or numbness in the legs, feet, or buttocks, exacerbated by walking or standing and relieved by sitting or bending forward.
Cervical stenosis may present with similar symptoms in the arms and hands and can sometimes lead to more severe issues such as difficulties with balance, coordination, and in extreme cases, bowel or bladder dysfunction. The latter indicates a serious condition called cauda equina syndrome, which requires immediate medical attention.
Symptoms can be intermittent or progressive, and in some individuals, spinal stenosis may be present without manifesting any noticeable discomfort. However, it is the recognition of these symptoms that prompts individuals to seek medical advice and potentially prevent further nerve damage or deterioration.
What are the Final Stages of Spinal Stenosis?
One question that often arises in my consultations is about the progression of spinal stenosis. While the trajectory can vary, the final stages of spinal stenosis are typically marked by increased severity and frequency of symptoms. In these stages, individuals may experience chronic pain that significantly interferes with daily activities, persistent numbness or weakness in the extremities, and, in severe cases, loss of bladder or bowel control.
It’s important to note that reaching these final stages is not inevitable. With early detection and appropriate management, many individuals with spinal stenosis can maintain a good quality of life. However, for those who do experience advanced symptoms, it becomes increasingly urgent to explore diagnostic and therapeutic options to alleviate their condition.
How is Spinal Stenosis Diagnosed?
Diagnosing spinal stenosis involves a combination of clinical evaluation and imaging studies. Initially, a thorough medical history and physical examination are performed, focusing on neurological assessment to pinpoint the affected area of the spine.
Imaging studies play a pivotal role in diagnosis. Magnetic resonance imaging (MRI) is often the tool of choice, providing detailed images of both bone and soft tissues, including the spinal cord and nerve roots. Computed tomography (CT) scans, especially when coupled with a myelogram (a contrast dye injected into the spinal column), can offer additional information on the extent and location of the stenosis.
In some cases, electromyography (EMG) and nerve conduction studies are used to evaluate the electrical activity of muscles and the speed of nerve signal transmission. These diagnostic tools collectively contribute to a comprehensive understanding of the individual’s condition, paving the way for targeted treatment strategies.
What is the Best Painkiller for Spinal Stenosis?
Pain management is a critical component of living with spinal stenosis. When it comes to medication, the “best” painkiller can vary based on the individual’s specific symptoms, overall health, and the underlying cause of their stenosis. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce inflammation and alleviate pain. However, they must be used cautiously due to potential side effects, especially with long-term use.
For more severe pain, doctors may prescribe stronger medications such as opioids, but these come with a high risk of dependency and other side effects. Muscle relaxants and anti-seizure drugs can also be effective in managing certain types of pain and muscle spasms associated with spinal stenosis.
In my experience, a comprehensive approach that also includes physical therapy, exercise, and lifestyle modifications often yields the best outcomes. It is also essential to consult with a healthcare professional before starting any pain management regimen to ensure it is appropriate for your specific circumstances.
Spinal Stenosis Treatment Options: An Overview
When it comes to spinal stenosis treatment, there is no one-size-fits-all approach. Treatment plans are tailored to the individual’s symptoms, the severity of the stenosis, and their overall health. Conservative treatments are typically the first line of defense, including physical therapy, pain medication, and corticosteroid injections that can help to reduce inflammation and pain.
For those who do not find sufficient relief from conservative measures, more invasive options may be considered. These can range from minimally invasive procedures, such as decompression techniques, to more extensive surgeries like laminectomy or spinal fusion.
In parallel with medical treatments, lifestyle modifications can also play a significant role in managing symptoms. Weight loss, regular exercise, and ergonomic adjustments can all contribute to reducing the strain on the spine and improving overall spine health.
Newest Treatments for Spinal Stenosis
The landscape of spinal stenosis treatments is continually evolving, with new therapies emerging that offer hope for improved outcomes. One of the latest advancements is the use of interspinous spacers, devices implanted between the vertebrae to open up the space around the nerves without the need for more invasive surgery.
Regenerative medicine techniques, such as stem cell therapy and platelet-rich plasma (PRP) injections, are also being explored as potential treatments to promote healing and reduce inflammation. While these newer treatments show promise, it is essential to consult with a healthcare professional to understand their risks, benefits, and suitability for your specific situation.
Surgical Solutions: Spinal Stenosis Surgery
For some individuals, surgery becomes a necessary option to relieve the symptoms of spinal stenosis. The most common surgical procedures include laminectomy, where a portion of the vertebra is removed to create more space for the nerves, and foraminotomy, which widens the openings for nerve roots.
In certain cases, a spinal fusion may be performed to stabilize the spine if there is significant instability or deformity. While these surgeries can be quite effective, they are not without risks, and the recovery process can be lengthy. Therefore, surgical solutions are generally considered only after conservative treatments have failed to provide adequate relief.
Non-Surgical Approaches to Spinal Stenosis: Medication and Exercises
Many individuals with spinal stenosis find relief through non-surgical approaches. Medications ranging from over-the-counter pain relievers to prescription drugs can play a vital role in managing pain and inflammation. Additionally, a targeted exercise program can help to strengthen the muscles supporting the spine, improve flexibility, and reduce pressure on the nerves.
Physical therapy often includes a combination of stretching, strengthening, and aerobic exercises, tailored to each individual’s condition. It’s important to work with a professional to ensure that exercises are performed correctly and safely to avoid exacerbating symptoms.
Tips for Spinal Stenosis Self-Care
Self-care is an integral part of managing spinal stenosis. Simple strategies can include maintaining a healthy weight, practicing good posture, and using heat or cold therapy to alleviate pain. It’s also beneficial to engage in regular low-impact activities, such as walking or swimming, to maintain mobility and spine health.
For those who spend many hours sitting, ergonomic adjustments to the workspace can reduce strain on the spine. Additionally, avoiding activities that exacerbate symptoms, such as heavy lifting or repetitive motions, can help to manage discomfort and prevent further injury.
Conclusion: Living with Spinal Stenosis
Living with spinal stenosis can be challenging, but with the right knowledge and treatment plan, it is possible to manage symptoms and maintain a fulfilling life. Understanding the causes and symptoms, exploring the range of treatment options, and committing to self-care can all contribute to a better quality of life.
If you or a loved one are grappling with spinal stenosis and have not found relief from traditional treatments, it may be time to consider other options. Dr. Rosenstein’s expertise in spinal conditions offers a beacon of hope for those seeking reprieve from their discomfort. It’s worth a consultation to see if you are a candidate for surgery to correct the issues causing you discomfort. Contact us today and take the first step toward reclaiming your comfort and well-being.
